
Services

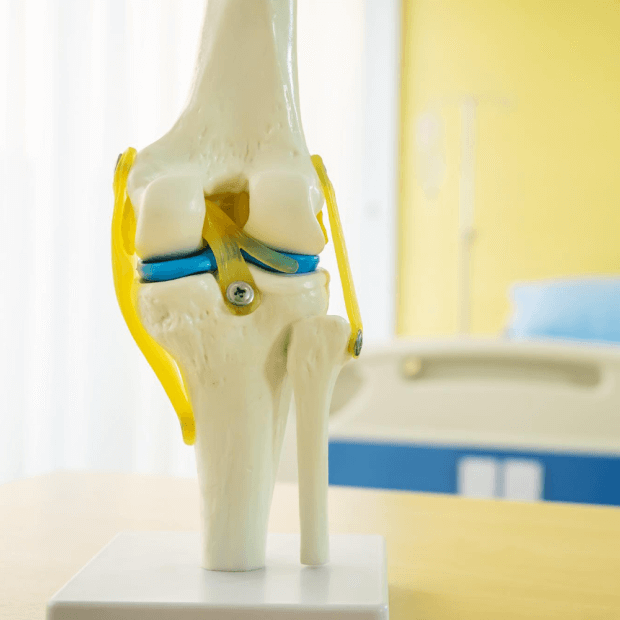
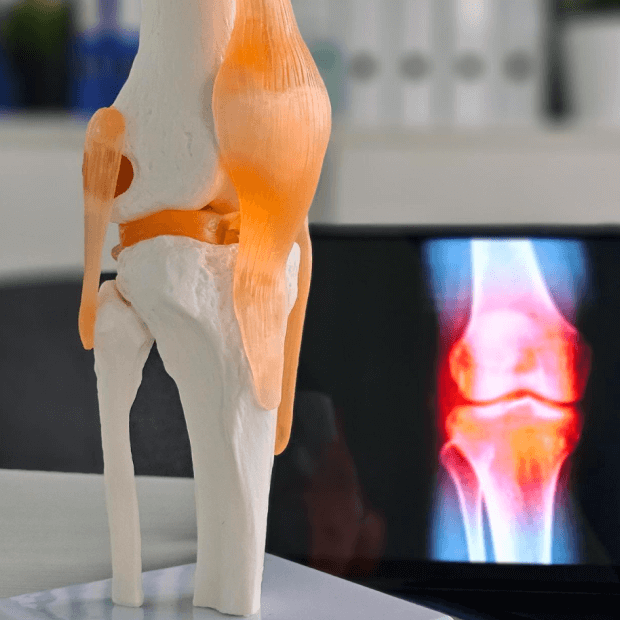
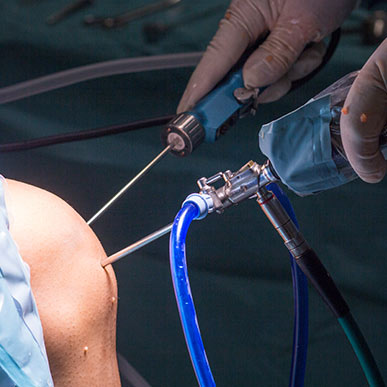
Cartilage Surgeries
I firmly believe in the power of nature and the natural laws of the body. I offer a unique approach to creating a complete and personalized path to wellness.
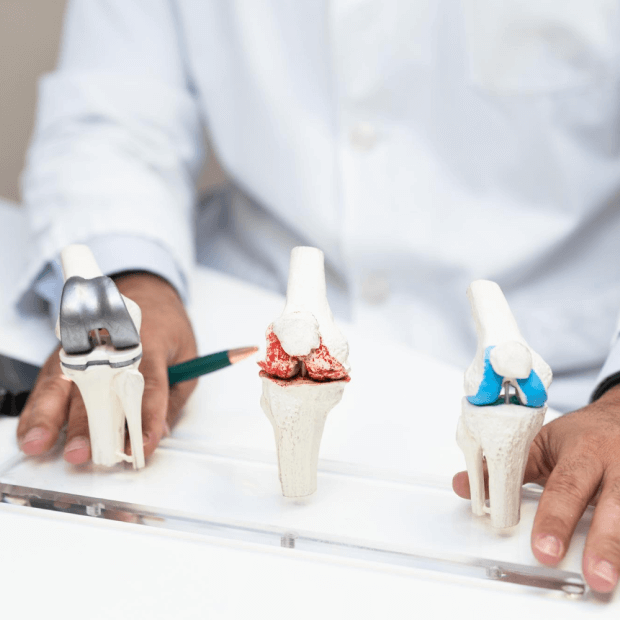
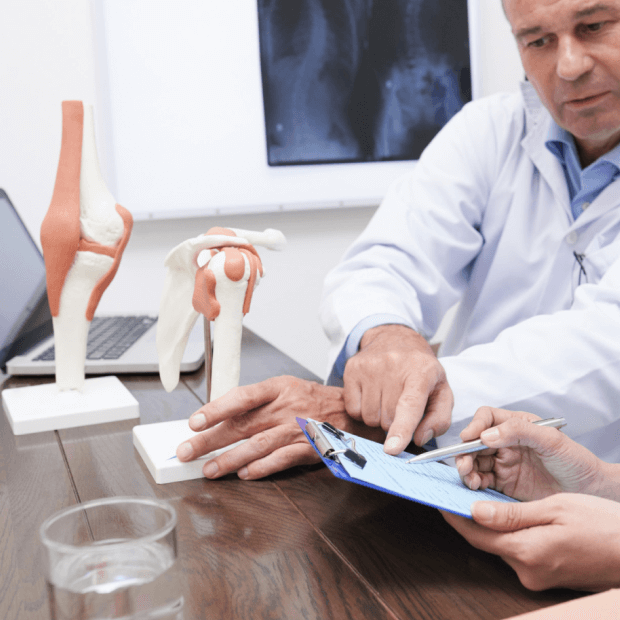
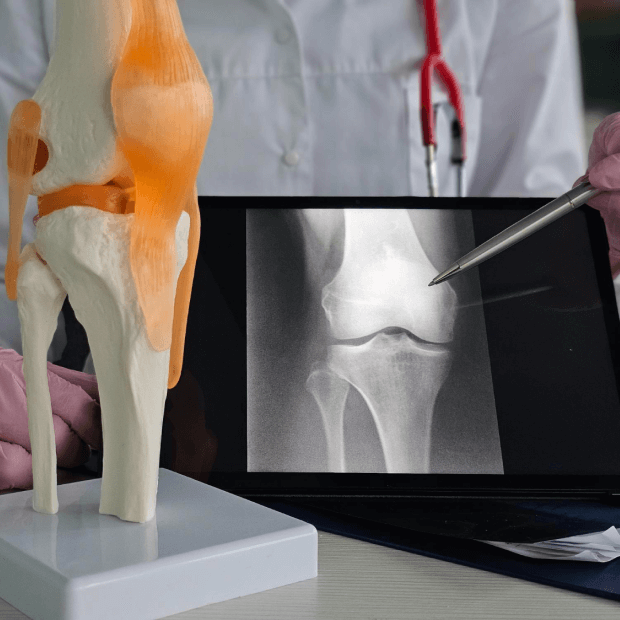
Joint Replacements- Hip, Knee and Shoulder
Joint replacement surgeries are advanced orthopedic procedures designed to relieve pain, restore mobility, and improve quality of life in patients suffering from severe joint damage due to arthritis, trauma, or degenerative conditions. With extensive training and experience in complex joint replacements, Dr. Rohit V specializes in knee, hip, and shoulder replacements, offering patients state-of-the-art surgical care tailored to their needs.
Cartilage Repair and Regeneration
Cartilage surgeries are specialized procedures aimed at repairing or regenerating damaged joint cartilage. Since cartilage has minimal ability to heal on its own due to poor blood supply, surgical intervention becomes essential for patients with cartilage defects, injuries, or early degenerative changes. These procedures help restore smooth joint surfaces, preserve joint health, and delay the progression of arthritis. Depending on the size and location of the defect, techniques may include microfracture, osteochondral grafting, autologous chondrocyte implantation (ACI), or biologic augmentation with stem cells and PRP.
When Is Cartilage Recommended?
- Young to middle-aged patients with focal cartilage defects
- Athletes and active individuals seeking to preserve joint function
- Patients with cartilage damage due to injury, wear, or early degeneration
- Individuals with persistent pain or swelling unresponsive to conservative treatment
- Cases where joint preservation is preferred over joint replacement

Benefits Cartilage Surgeries
- Relieves pain and improves joint function
- Restores normal joint mechanics and mobility
- Prevents or delays the development of osteoarthritis
- Enhances long-term knee and hip health
- Helps athletes and active individuals return to sports and physical activity
- Minimally invasive options allow faster recovery with fewer complications
More Services
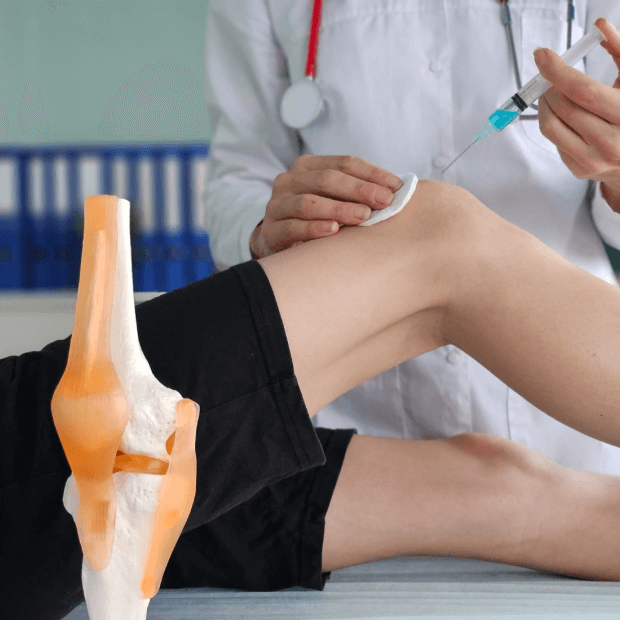
PRP Injection
PRP injection is an advanced regenerative treatment that uses the body’s own healing potential to repair injured tissues, reduce pain, and promote recovery. The procedure involves drawing a small sample of the patient’s blood, processing it to concentrate the platelets and growth factors, and injecting the platelet-rich plasma directly into the affected area under ultrasound or guided precision. These bioactive components stimulate tissue regeneration, enhance collagen production, and improve blood supply to the injured site.
PRP therapy is commonly recommended for patients with chronic tendon injuries, mild to moderate osteoarthritis, ligament sprains, sports injuries, and even post-surgical recovery to accelerate healing. Compared to conventional treatments, PRP offers a natural, minimally invasive solution with reduced downtime and longer-lasting results.

BMAC injection
BMAC injection is a cutting-edge regenerative therapy that utilizes stem cells and growth factors derived from the patient’s own bone marrow to promote healing and tissue regeneration. The procedure involves aspirating bone marrow, usually from the pelvic bone, and processing it to concentrate mesenchymal stem cells, platelets, and cytokines. This concentrate is then injected into the affected joint, tendon, or cartilage defect under precise image guidance. The biologically active components in BMAC stimulate repair, reduce inflammation, and enhance the regeneration of damaged tissues.
BMAC therapy is particularly recommended for patients with early to moderate osteoarthritis, cartilage injuries, chronic tendon disorders, ligament injuries, and in certain cases as an adjunct to orthopedic surgeries. Compared to traditional treatments, BMAC offers a minimally invasive and natural alternative that can delay or even prevent the need for joint replacement surgery.
OATS procedure
The OATS procedure is an advanced cartilage restoration technique designed to treat focal areas of cartilage damage in the knee and other joints. It involves transferring healthy cartilage along with underlying bone (osteochondral plugs) from a non-weight-bearing area of the joint to the damaged region. This not only restores the cartilage surface but also provides structural support through the transplanted bone, allowing for more effective integration and long-term durability. By using the patient’s own tissue, the risk of rejection is eliminated, and the transplanted cartilage functions like native tissue, offering a natural repair.
Mosaicplasty
Mosaicplasty is a cartilage restoration surgery that involves transplanting multiple small cylindrical plugs of healthy cartilage and underlying bone from non-weight-bearing areas of the joint into a damaged region. These plugs are placed side by side in a mosaic-like pattern, hence the name, to cover the defect and restore a smooth joint surface. The transplanted cartilage integrates with the surrounding tissue, while the bone plugs provide stable anchoring and promote healing.
This technique is especially effective for treating small to medium-sized cartilage defects caused by injury or localized wear, particularly in younger and active patients. By using the patient’s own tissue, mosaicplasty eliminates the risk of graft rejection and ensures a biological, long-lasting repair.
Minced Cartilage Repair/ Reconstruction
Minced cartilage repair is an innovative, biological cartilage restoration technique that uses small fragments of healthy cartilage—harvested from low-load bearing areas of the joint—to repair damaged cartilage surfaces. These cartilage fragments are minced into tiny pieces and then implanted into the defect site, often combined with biological adjuncts such as fibrin glue, PRP (Platelet-Rich Plasma), or BMAC (Bone Marrow Aspirate Concentrate) to stimulate regeneration. The minced fragments release viable chondrocytes and extracellular matrix components, which contribute to new cartilage formation and integration with the surrounding tissue.

Osteochondral Allograft Transfer
Osteochondral allograft transfer is a cartilage restoration procedure where a fresh donor graft containing both viable cartilage and underlying bone is transplanted into a patient’s cartilage defect. This technique is particularly valuable for large, deep, or complex cartilage injuries where other repair methods may not be sufficient. The allograft provides mature, structurally intact hyaline cartilage along with healthy subchondral bone, which helps restore the joint’s natural anatomy and biomechanics.
Unlike autograft techniques such as OATS or mosaicplasty, OCA does not require harvesting from the patient’s own joint, thereby avoiding donor-site morbidity. The graft is precisely shaped to match the defect, ensuring optimal integration and stability.
Parapatellar Release
Parapatellar release, commonly referred to as lateral retinacular release, is a surgical procedure performed to correct patellar maltracking and relieve anterior knee pain caused by excessive lateral pull on the kneecap. In this technique, the tight lateral retinaculum—a band of fibrous tissue on the outer side of the knee—is carefully incised or released arthroscopically to allow the patella to realign more centrally within the femoral groove. This improves patellar tracking, reduces abnormal pressure on the cartilage, and helps alleviate pain during activities such as climbing stairs, squatting, or prolonged sitting.
The procedure is generally recommended for patients with symptomatic patellar tilt, recurrent lateral patellar compression syndrome, or instability that does not respond to conservative measures such as physiotherapy and bracing. When combined with rehabilitation, parapatellar release can enhance knee function and reduce discomfort.


Cuff Repair with Patch Augmentation
Patch augmentation is used to strengthen rotator cuff repairs, especially in large or complex tears. A biological or synthetic patch is applied over the repaired tendon, enhancing healing and providing additional support. This technique improves repair durability, reduces re-tear risk, and ensures better long-term shoulder function.
Advanced Cartilage Repair for Pain-Free Mobility

Joint Replacements
Advanced hip, knee, and shoulder joint replacements ensuring pain relief, improved mobility, and long-lasting recovery.

Arthroscopic Rotator Cuff Repair
MBBS, BPharm, FRCOG, FRANZCOG
Minimally invasive arthroscopic rotator cuff repair to relieve pain, restore shoulder strength, and improve mobility.
Arthroscopic Bankarts Repair
Minimally invasive arthroscopic Bankart’s repair to treat shoulder instability, restore joint stability, and prevent recurrent dislocations.

ACL Reconstruction
Advanced ACL reconstruction surgery to restore knee stability, support active lifestyles, and prevent future joint injuries.

Meniscal Repairs
Arthroscopic meniscal repair to preserve knee function, relieve pain, restore mobility, and prevent long-term joint damage.

Cartilage Surgeries
Specialized cartilage surgeries to repair joint damage, reduce pain, restore mobility, and protect long-term joint health.

High Tibial Osteotomy
High tibial osteotomy surgery to correct knee alignment, relieve arthritis pain, and preserve natural joint function.

Endoscopic Carpal Tunnel Release
Minimally invasive endoscopic carpal tunnel release to relieve wrist pain, restore hand function, and improve mobility.

